55% of postmenopausal women experience symptoms of vaginal dryness.1
Vaginal dryness can occur at any age due to several different causes, but it is mostly associated with a drop in oestrogen levels, a condition frequent in menopausal.2,3 Other oestrogen deficency states may affect cancer survivors, postpartum women and those who have been taking oral contraceptives for long time.2,3
Vaginal dryness is often accompanied by other symptoms like burning, irritation, dyspareunia, post-coital bleeding, vaginal bleeding, painful intercourse3 and increased risk for recurrent vaginal infections and urinary tract infections.2
1 Kingsberg SA,et al. Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women’s VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. J Sex Med. 2013
2Bleibel B, Nguyen H. Vaginal Atrophy. StatPearls 2021
2Nappi R.E. et al., Climateric 2020
The vulva hygiene is the first line of defence to protect from genital infections.1
Contaminants often collect in the vulvar folds. Increasing in moisture, sweating, menses and hormonal fluctuations influence vulvar microbial growth and species balance, potentially resulting in odour and vulvovaginal infection.
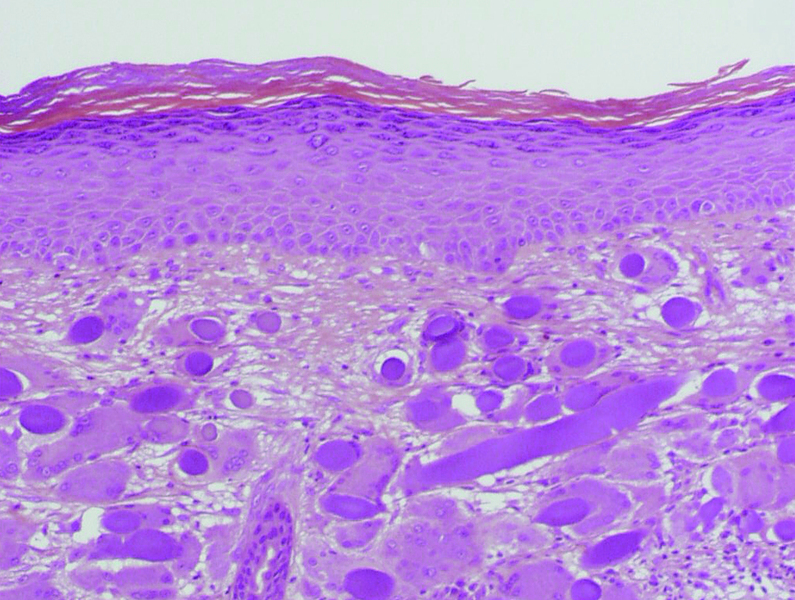
Genital skin is unique: it is covered by a thin stratum corneum, non-keratinized thus more permeable for microbial then the rest of body’s skin. Another characteristic of vulvar skin is the slightly more acidic pH compared to the rest of the body. Vulvar pH could be expected to fall between values of the skin and vagina’s pH (respectively, on average 4.7 and 3.5). For these reasons, it is advisable to take care of the vulvar skin by using intimate hygiene products that are specifically formulated and tested for this purpose.1
1Chen Y. et al. (2017) ‘Role of female intimate hygiene in vulvovaginal health: Global hygiene practices and product usage’, Women’s Health
The menopause transition is experienced by 1.5 million women in US each year and often involves troublesome symptoms.
The most proximity symptoms to menopause are vaginal dryness, hot flushes, mood swings and insomnia.1
Menopause is a complex period in women’s life. Several symptoms bear an obvious relationship to the changing hormonal milieu associated with menopause.
Symptoms related to menopause are vasomotor symptoms, difficulty sleeping/insomnia and adverse mood/depression. Hot flashes are reported by up to 85% of menopausal women and their incidence and severity increases as women traverse the menopause, peaking in the late transition and tapering off within the next several years. Sleep quality generally deteriorates with aging, and menopause seems to add an additional, acute layer of complexity to this gradual process. Studies indicate that as much as 25 minutes of sleep per night can be lost when a woman is premenstrual in her late reproductive years. An increased risk of depressed mood during the menopause transition and an approximately 3-fold risk for the development of a major depressive episode are shown during perimenopause.
Depressed mood, poor sleep and higher body mass index are interconnected and influence each other during menopause transition.1
1Santoro N. et al. (2015) ‘Menopausal Symptoms and Their Management’,Endocrinol Metab Clin North Am
Interstitial cystitis is not an infection.1 Interstitial cystitis can affect women but also men with an impaired related Quality of Life.2
Interstitial cystitis is an alteration of the internal mucous layer of the bladder where the epitelial cells are in direct contact with the urea, resulting in a chronic inflammation.1 The prevalence ranges from 0.44% in Europe to 0.87% in US.2,3 It can be confused with an urinary infection carring similar symptoms, thus be diagnosed late.1,4 Patients often describe pain in the bladder region, with an urge to urinate. This sensation is worsened with the filling of the bladder and is often relieved by urinating more often. This may happen during the daytime and/or during the night. Other symptoms, such as pain or discomfort while urinating and pain or discomfort during sexual intercourse, may be present. This condition report a negative effects on relationships and emplyment, and significant more sleep dysfunction, depression, anxiety and stress.1,4
1EAU-Guidelines-on-Chronic-Pelvic-Pain-2023 https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Chronic-Pelvic-Pain-2023.pdf
2 Anger J.T., National prevalence of IC/BPS in women and men utilizing veterans health administration data, Frontiers in Pain Research, 2022
3Hakimi Z., et al., The Burden of Baldder Pain in 5 European Countries: a cross sectional study Urology 2016
4MacDiarmid S.A.Diagnosis of Interstitial Cystitis/Painful Bladder Syndrome in Patients With Overactive Bladder Symptoms,2007 MedReviews
Neurological disorders affect up to one billion people worldwide.1
Neuroendocrine disorders are related to a variety of behavioural symptoms such as weakness and fatigue, depressed mood, lack of motivation, decreased performance at work and in sport, decreased vitality, increased anxiety and irritability, insomnia, difficulty concentrating and impaired memory.2
Metabolic alteration of neurons and neurotrasmitters contribute to develop depression and stress related disorders. The World Health Organization (WHO) has ranked depression the 4th leading cause of disability worldwide and projects that by 2030, it will be the first leading cause.3 Modern technologies highlighted both the crucial role played by membrane phospholipids in ensuring optimal neuronal function in the adult brain and the relative loss of their efficacy during the ageing process.2
1https://www.who.int/news/item/27-02-2007-neurological-disorders-affect-millions-globally-who-report#:~:text=Neurological%20disorders%20also%20include%20brain,from%20Alzheimer%20and%20other%20dementias
2Biggio 2020
3Biggio 2018
About 2.4 percent of the population is affected by peripheral neuropathy and the prevalence increases to 8 % in older population.1
Peripheral neuropathies encompass disorders of peripheral nerve cells and fibers, which manifest secondary to a wide range of pathologies. The most frequently encountered symptoms of peripheral neuropathy include numbness and paresthesias; pain, weakness, and loss of deep tendon reflexes may accompany these symptoms. Peripheral neuropathies usually develop over months to years, while some may develop more rapidly and be progressive in nature. Peripheral neuropathies have a broad range of severity and clinical manifestations, as they can affect motor, sensory, and autonomic fibers.
1Neuropathy, C Hammi, Yeung. StatPearls Publishing; 2023 Jan.
Chronic inflammatory disaeses are the most significant cause of death in the world.1
Inflammation is part of the body’s defense mechanism by which the immune system recognizes and removes harmful and foreign stimuli and begins the healing process. Inflammation can be either acute or chronic. Tissue damage due to trauma, microbial invasion, or noxious compounds can induce acute inflammation. It starts rapidly, becomes severe in a short time and symptoms may last for a few days.
Chronic inflammation is also referred to as slow, long-term inflammation lasting for prolonged periods of several months to years. Generally, the extent and effects of chronic inflammation vary with the cause of the injury and the ability of the body to repair and overcome the damage.1
1Pahwa R, Goyal A, Jialal I. Chronic Inflammation. [Updated 2023 Aug 7]. In: StatPearls [Internet]
1G. Cooper, B. Stroehla: The epidemiology of autoimmune diseases; Autoimmun Rev , 2003; 2(3):119-25
2GBD 2021 Osteoarthritis Collaborators,Global, regional, and national burden of osteoarthritis, 1990–2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021,The Lancet
3Nagy H, Carlson K, Khan MAB. Dysmenorrhea. [Updated 2023 Nov 12]. In: StatPearls [Internet]
Related areas